Total Body Photography and its Use in the High-Risk Melanoma Patient
The incidence of melanoma in the United States has been rising for at least 30 years. Currently, the lifetime risk of acquiring melanoma is about 2.4% (1 in 40) for Caucasians, 0.5% (1 in 200) for Hispanics and 0.1% (1 in 1000) for African Americans. When diagnosed before spread of the tumor to regional lymph nodes or organ systems, the overall 5-year survival rate for melanoma patients in the US is about 98%. For disease that has advanced to the lymph nodes, the survival rate falls to 63%, and it is only 16% when metastasis to distant organs has occurred.
Many individual risk factors for cutaneous melanoma have been identified, including personal or family history of melanoma, presence of atypical nevi, and a large number of nevi. Patients with a history of one melanoma are at 9-fold increased risk of developing a second melanoma compared to the general population. Routine skin cancer screening of such high-risk individuals may help detect melanomas when they are thin and lead to increased survival. Obtaining a skin biopsy and histologic examination of suspicious lesions remains the gold standard for diagnosing melanoma, but in an attempt to reduce the number of unnecessary biopsies, several noninvasive modalities have been suggested.
Most early melanomas exhibit observable change over a period of months (reflected by the addition of the letter 'E' for 'Evolving' to the ABCDE acronym [asymmetry, border, color, diameter] for melanoma detection). Digital or print photography can aid the examiner in detecting concerning changes by providing side-by-side comparisons at two points in time. Close-up dermatoscopic photography can help in monitoring pre-existing nevi.
However, up to 19% of melanomas diagnosed in a high-risk cohort monitored with total body photography (TBP) were biopsied because they were new lesions, paralleling the observation that melanoma more often develops de novo in clinically normal-appearing skin rather than in pre-existing melanocytic nevi. TBP, in which baseline regional photographs are taken of patients in standardized poses, captures existing nevi and surrounding 'nevus-free' areas of skin simultaneously. Such photographs may be archived electronically in a patient's chart for comparative use at follow-up screening exams. They may also be provided to the patient to aid in between-appointment self-screening exams. While one of the strengths of TBP lies in its ability to detect new lesions, depending on the resolution of the clinical photographs, changes may be captured in existing nevi as well. See Figures 1 and 2 below, demonstrating the use of TBP in identifying the development of melanomas.
Figure 1. 23-year-old female with history of melanoma. TBP performed shortly after melanoma diagnosis. Compared with baseline (left), follow-up TBP (right) revealed the enlargement of a nevus (mildly dysplastic on histology). Images courtesy of Dr. Stephanie Savory.
Figure 2. Male with extensive personal and familial history of melanoma. Compared with baseline TBP (left), 6-month TBP revealed the development of a melanoma (prominent central pigment, flanked by a pink and white patch). This was an invasive melanoma (0.25 mm). Images courtesy of Dr. Stephanie Savory.
When high-risk patients were monitored with either TBP or serial dermoscopy, TBP was associated with lower biopsy rates and higher melanoma detection rates, suggesting that TBP is better able to detect de novomelanomas. Serial dermoscopy may be superior in tracking dysplastic nevi, a very small percentage of which progress to melanoma. It has been estimated that the lifetime rate of an individual mole on a 20-year-old transforming to melanoma by 80 years is 0.03% in men and 0.009% in women. The best use of TBP in monitoring high-risk patients may be in combination with dermoscopy to allow detection of new melanomas and changes in existing dysplastic nevi, a technique Salerni, et al. calls the 'two-step' method. Using the combined approach, Wang, et al. reports that all melanomas diagnosed in a high-risk cohort over a 10-year period were either in situ or less than 1 mm. There were no instances of metastatic melanoma or melanoma-related deaths.
The main goal of TBP is melanoma detection at an early disease stage, which translates to higher survivability. Reduction of unnecessary biopsies is a secondary endpoint. While stringent, randomized controlled trials are lacking, data suggest TBP achieves these goals. In addition, TBP may be more useful when used for long-term monitoring. A retrospective chart review of patients in their first year of care at a sub-specialty pigmented lesions clinic compared biopsy number in patients with multiple atypical nevi receiving total body skin exam with those receiving TBP plus total body skin exam, and failed to show a difference. A subgroup of melanoma may be slow growing, and in the 10-year experience of Salerni, et al., can be diagnosed at any time in the follow-up period, suggesting that in a high-risk cohort, use of TBP for long-term monitoring is most appropriate.
TBP may be most useful in older patients in whom new or changing lesions are more likely to be melanoma. In their cohort study of patients at high risk for melanoma undergoing screening with dermoscopy and TBP, Banky, et al.noted that in patients younger than 50 years, less than 1% of all new lesions and 3% of changed lesions were melanomas, whereas in patients older than 50 years, 30% of new lesions and 22% of changed lesions were melanoma. Longitudinal monitoring with TBP may also reduce cancer anxiety in certain subsets of high-risk patients, especially those with a personal history of melanoma.
Despite the apparent benefits of TBP in terms of advanced melanoma detection, particularly when coupled with dermoscopy and total-body skin exam, conclusive data showing a reduction in morbidity and mortality are lacking. The absence of a suitable control group also makes the completion of a more rigorous trial to determine optimal screening in high-risk patients difficult.
A significant limitation of TBP is cost, which can be as high as $500 per person for the photographs, and it is not typically covered by insurance. Additionally, total-body skin examination in a high-risk individual using TBP can be laborious and time consuming. Computerized imaging technologies are available to help clinicians streamline the examination process. Some compare baseline photos with those taken at follow-up visits to aid in the detection of new lesions. Many also include an algorithmic scoring system designed to alert the clinician to lesions of concern. However, rigorous independent studies validating the accuracy of these systems are not available.
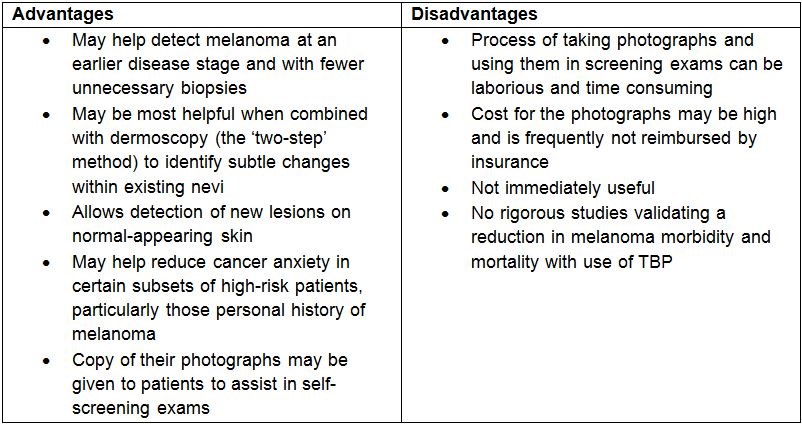
Table 1. Advantages and disadvantages to use of TBP for monitoring patients at high risk of developing melanoma
In summary, total body photography may be most helpful in identifying new and changing nevi in a subset population of patients at high risk for developing melanoma. Its accuracy may be improved with the concurrent use of dermoscopy. Practical downsides to the use of TBP are that its use can be time-consuming, and most insurance networks do not cover its reimbursement. Additionally, data from rigorous controlled trials is lacking.


