Photodynamic therapy for photoaging
Aging is a complicated and multifactorial process that happens in all individuals at a variable rate, affected by environmental, hormonal, and genetic factors, which result in several functional and aesthetic changes in the skin. Photoaging is manifested clinically by fine and coarse wrinkling, roughness, dryness, laxity, sallowness, pigmentary mottling, telangiectasia, and, in some cases, pre-neoplastic and neoplastic lesions.
UV radiation increases the levels of matrix metalloproteinases (MMPs) in human skin, which are the enzymes responsible for the degradation of extracellular matrix proteins, such as collagen type I and III. MMP-1 is the main enzyme that degrades collagen in the skin, and once MMP-1 breaks down collagen, further degradation is followed by MMP-3 and MMP-9.
The term 'photodynamic therapy' was introduced by Professor Hermann von Tappeiner, in 1903, to describe the application of a photosensitizer followed by light in the presence of oxygen. By the early 1990s, Kennedy et al reported the use of topical aminolevulinic acid to treat actinic keratosis (AK). Many years later, it was possible to show improvement in photoaging skin when using photodynamic therapy (PDT) to treat field cancerization. In 2003, Touma and Gilchrest reported improvement in skin quality, fine wrinkles and sallowness. Similarly, Ruiz-Rodriguez et al noted attenuation of photodamaged skin associated with a reduction in the number of AK lesions after aminolevulinic acid (ALA)-PDT and intense pulsed light.
PDT treatment protocol is established for non-melanoma skin cancer and field cancerization. In addition, several different protocols are reported for photorejuvenation. The two main photosensitizers are ALA and methyl ester ALA (MAL). The published studies on skin rejuvenation usually employ different sources of light, such as intense pulsed light (IPL), light emitting diode (LED) and laser.
PDT with IPL
IPL devices are used for full-face treatment for photodynamic rejuvenation, particularly in the USA and Brazil. Diverse parameters of IPL with respect to wavelength, pulse duration, pulse interval, and energy density have been used for PDT treatment. The superior efficacy of IPL in combination with a photosensitizer (ALA or MAL) as opposed to sole IPL treatment has been demonstrated in numerous studies in split-face comparison. In PDT, handheld devices with a cut-off filter that allow transmission of light above about 600 nm are typically suitable. In comparison, to continue irradiation with red light, PDT with a flash lamp is perceived to be less painful. In many studies, with different protocols, improvement of signs of skin aging, such as hyperpigmentation, tactile roughness, telangiectasia, and wrinkles has been reported. Nonetheless, to date, no clearly defined treatment parameters for PDT with IPL exist.
PDT with red light
Some studies have demonstrated the efficacy of PDT with red light in the treatment of photo-induced skin aging. Significant improvement in mottled hyperpigmentation fine lines, roughness, sallowness, AK lesions, and laxity are reported. Issa et al reported improvement of wrinkles, skin texture, skin coloration, and clearance of AK after two sessions of MAL-PDT with red light (37 J/cm2), and the results were even better at the second follow-up after 6 months, at which further improvement in laxity was observed (Figure 1). Moreover, the authors reported marked global clinical improvement as well as skin remodeling in patients with or without clinically-evident AK lesions.

PDT with blue light
Protoporphyrin IX (Pp IX) has an absorption maximum at 410 nm; for this reason, blue light (420-490 nm) is about 50 times more effective in the activation of Pp IX than red light (590-750 nm), which uses the small absorption peak of Pp IX at 635 nm. The main disadvantage of blue light is its shorter wavelength, which results in a reduced depth of penetration in skin: 1-2 mm for blue light versus about 4 mm for red light. However, many studies confirm the efficacy of PDT with blue light in the treatment of skin aging, including not only improvement in AK lesions, but also in the skin texture, elasticity and pigmentation. The efficacy of MAL-PDT independent of the wavelength employed (blue vs red light) was compared in a split-face study, and no difference with respect to improvement of photodamaged skin was observed.
PDT with pulsed dye lasers (PDL)
PDT with PDL has proved its efficacy in the treatment of AK with the advantage of reduced painfulness. These lasers are also employed for photodynamic skin rejuvenation. PDT with PDL is well suited for the treatment of the vascular component of photodamaged skin that responds less well to PDT and red light.
Histologic analysis and mechanism of action
Our understanding of the possible mechanisms of action of PDT for skin rejuvenation has continued to advance in recent years. Park et al investigated whether ALA-PDT-induced histologic changes resulted in photorejuvenation. After two sessions, at one-month intervals, the mean epidermal thickness and dermal inflammatory infiltrate were reduced. The total collagen volume in the dermis significantly increased with expression of type I and II procollagen and the level of transforming growth factor β (TGF β) and TGF type II receptors in the epidermis also increased. The elastic material with co-localizing fibrillin-1 and tropollastin expression in dermis decreased after treatment, and the expression of MMP -1, -3 and -12 also decreased one month after treatment.
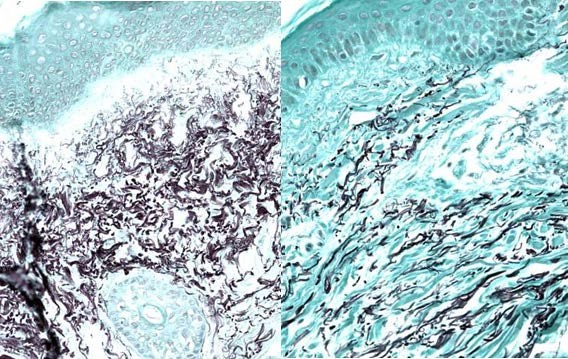
Issa et al evaluated skin remodeling induced by MAL-PDT in photodamaged skin by immunohistochemical studies (collagen types I and III; MMP-1, -3, -7, -9, -12; and TIMP-1 [tissue inhibitor of MMP]). Skin biopsies were performed before, and at three and six months after treatment. A significant increase in expression of MMP-9 in the dermis was detected at three months after treatment. Significant increases in the expression of collagen type I at three and six months were also observed. Issa et al also evaluated histopathologic changes induced by MAL-PDT and morphometrically quantified collagen and elastic fibers (Figures 2 and 3) in skin remodeling by MAL-PDT in photodamaged skin before, and three and six months after treatment (two sessions with a four-week interval). They reported the decrease in the amount of elastic fiber three and six months after treatment, showing that the increase in the amount of collagen fiber was statistically significant after six months of treatment. Histopathologic and morphometric results were consistent with the clinical findings in this study.
Szeimies et al evaluated clinical, histological and immunohistochemical changes in human skin with field cancerization after three sessions of MAL-PDT with AK clearance. A significant reduction in the degree and extent of keratinocyte atypia was observed. Also, a significant increase in collagen deposition and improvement in solar elastosis were noticed after three months of treatment. Immunohistochemistry showed only a trend for decreased TP-53 expression, increased procollagen I and MMP-1 expressions and an increased expression of tenascin.
Bagazgoitia et al reported expression of p53, an early marker of epidermal carcinogenesis that is not expressed in normal skin, which was significantly reduced after PDT. The authors conclude that PDT can reverse the process of carcinogenesis in photodamaged skin.
Molecular mechanism of skin rejuvenation: discussion
We are still far from a thorough explanation of the molecular mechanism of skin rejuvenation induced by PDT. Despite this, many studies have advanced our understanding in this field.
Skin extracellular matrix (ECM) is a complex network of macromolecules secreted by cells and is responsible for many cellular transduction signals. MMPs are extracellular proteolytic enzymes capable of digesting various structural components of the ECM, and are directly involved in dermal remodeling. Many cytokines and growth factors, such as TGF-β, TNF-α, interferon and IL-1 are able to regulate the transcription of MMPs. The presence of reactive oxygen species, generated by solar irradiation or phototherapy has an important role in the regulation of these enzymes. PDT can increase both expression and enzymatic activity of MMP-9 in mouse tumors. PDT also involves the influx of MMP-9 expressing inflammatory host cells.
Kobayashi et al investigated the pathophysiological role of fibroblasts in tissue metabolism, analyzing gelatin-degrading enzymes secreted from skin cells in culture by zymography. MMP-2 was secreted from fibroblasts, whereas both MMP-2 and MMP-9 were secreted from keratinocytes. MMP-9 production was induced by addition of TGF-β or TNF-α to the cultures. Both MMP-2 and -9 secreted from fibroblasts could play important roles in tissue metabolism. Additionally, inflammatory mediators (IL-1, -2, -6, -8, -10 and TNF-α) have been reported to be modulated by PDT, which could induce MMP-9 expression in fibroblasts.
Some authors have speculated that PDT may induce an inflammatory response in photodamaged skin, with subsequent dermal remodeling by a paracrine pathway. They suggest that MAL-PDT could induce MMP-9 to degrade the fragmented elastic fibers and degenerated collagen (gelatin) into small fragments of proteins, therefore reorganizing the ECM, and inducing fibroblasts to synthesize collagen.
Light source | Photosensitizer | Number of sessions (interval) | Good results for |
PDT with IPL | ALA or MAL | 1-3 sessions (4 weeks) | Hyperpigmentation, telangiectasias, fine lines |
PDT with red light (LED) | Usually MAL | 2-3 sessions (4 weeks) | AK, hyperpigmentation, fine lines, deep wrinkles and laxity |
PDT with blue light (LED) | Usually ALA | 2-3 sessions (4 weeks) | AK, hyperpigmentation, fine lines, skin texture |
PDT with dye laser | ALA or MAL | 1-2 sessions (4 weeks) | AK, skin texture and vascular components of photodamaged skin |
Table 1. Photodynamic therapy for skin rejuvenation.
Effects of PDT are not limited to the site where photosensitization takes place, but are propagated in a chain reaction. EMC components are affected even when they are not the primary targets, and EMC-cells and cell-cell interactions are modulated as a result of photosensitization. Besides the selectivity of PDT, the modulation of EMC components and molecules of the immune system can be responsible for skin remodeling in the absence of tumor tissue.
Conclusion
PDT has shown strong efficacy and high tolerability for the treatment of non-melanoma skin cancer. More recently, PDT has been used widely, and with great success, for many off-label conditions, in addition to its use in cosmetic dermatology, notably photorejuvenation. The utility of PDT for photoaging treatment is apparent, but its mechanism of action has not been completely clarified. Some mechanisms involve in skin remodeling after PDT, such as cytokines induction, MMP expressions, solar elastosis reduction, and finally, collagen production. While therapy protocols in the treatment of skin cancers have been clearly defined, the treatment parameters for rejuvenation are not yet standardized and vary between the different studies. However, when treating aging skin associated with AK lesions, it is recommended to employ the standard protocol for AK, to guarantee effective treatment.
