Elbow instability injuries require evaluation strategy
 Elbow stability involves complex interactions among the bony articulation of the elbow joint, capsular ligamentous structures, and dynamic muscle restraints. Elbow instability may result in injuries. They often are chronic overuse injuries that occur with overhead throwing in athletes. Instability may affect the lateral or medial aspect of the elbow.
Elbow stability involves complex interactions among the bony articulation of the elbow joint, capsular ligamentous structures, and dynamic muscle restraints. Elbow instability may result in injuries. They often are chronic overuse injuries that occur with overhead throwing in athletes. Instability may affect the lateral or medial aspect of the elbow.
Understanding the functional anatomy of the elbow and the relative contributions to instability of the various structures is crucial to developing a strategy for diagnosis and management of injuries and recognizing the patient’s activity level requirements.
Anatomy and biomechanics
The anatomy of the elbow features several prominent characteristics.
Bony articulation. The radiohumeral and proximal radioulnar articulations allow for rotation or pivoting motion or both. The ulnohumeral articulation functions more as a hinge in forward flexion and extension. The greater sigmoid notch of the ulna articulates with the spool-shaped trochlea of the distal humerus to form a highly conforming articulation. The capitellum is aspheroidal; it is separated from the trochlea by a groove in which the radial head articulates. The radial head is concave and usually is more elliptical than circular; it is slightly offset from the neck.
Bony stability. The ulnohumeral articulation provides the elbow with a significant amount of inherent stability because of its congruent nature. As a result, the elbow has been considered primarily a hinge-type joint. The ulnohumeral joint may be assumed to move in a uniaxial articulation except when it is in extreme flexion-extension.
With the elbow in full extension, valgus instability is divided equally among the medial collateral ligament (MCL), anterior capsule, and bony articulation. The joint articulation provides about 55% of stability in extension and up to 75% in 90º of stability in flexion.1 At 90º of flexion, valgus instability does not change with the contribution of the articulation. These values represent a pure varus and valgus instability and do not take into account any rotational forces that usually are present with instability.
After a simple elbow dislocation, the olecranon process provides a significant amount of varus and valgus instability. Studies have shown that excision of the olecranon process leads to a decrease in combined stability in extension and at 90º of flexion.2
Posterior-directed forces are resisted by the coronoid process, which provides an anterior bony buttress. A correlation between coronoid fracture or fragment size and the tendency toward dislocation is particularly evident in the absence of a radial head.3
The importance of the radial head in elbow stability has received increasing recognition in recent years. Studies have shown that the radial head can provide as much as 30% of valgus stability, even when the MCL is intact. If the MCL is disrupted, the radial head becomes a crucial secondary elbow stabilizer and provides up to 75% of the resistance to valgus stress. In addition, about 60% of longitudinally applied force normally is transmitted through the radial head.
Capsule. When taut in extension, fibrous bands within the elbow joint provide significant strength and an important stabilizing effect. The anterior capsule may be a significant stabilizing element to pure varus and valgus stress in extension but not in flexion.
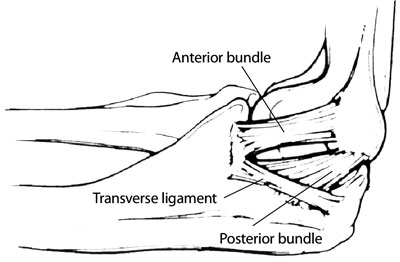
Medial collateral ligament. The MCL complex, also known as the medial ulnar collateral ligament (MUCL), consists of three bundles: anterior, posterior, and transverse (Figure 1). The anterior bundle is the strongest component of the MUCL. It originates in the anteroinferior aspect of the medial epicondyle and inserts onto the medial aspect of the coronoid process at the sublime tubercle, with an average distance of 18 mm distal to the coronoid tip.
The anterior bundle is functionally composed of an anterior band and a posterior band that provide resistance in valgus stress throughout the range of flexion and extension motion. The posterior bundle is a fan-shaped thickening of the capsule that originates on the medial epicondyle and forms the floor of the cubital tunnel. The transverse ligament connects the inferomedial coronoid process with the medial tip of the olecranon. It is thought to make little or no contribution to valgus stability.4
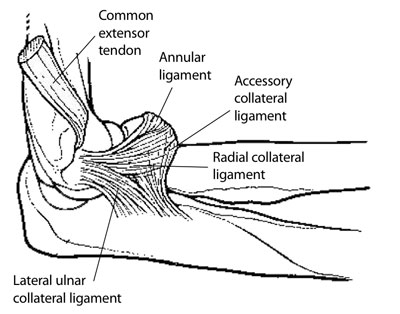
Lateral collateral ligament. The lateral collateral ligament (LCL) complex has four components: annular ligament, radial collateral ligament (RCL), lateral UCL (LUCL), and accessory LCL (Figure 2). This complex originates from the lateral epicondyle at a point through which the center of rotation passes; therefore, it is isometric throughout the normal range of flexion-extension. The RCL terminates in the annular ligament, which stabilizes the proximal radioulnar joint. The LUCL, which is superficial and distal, inserts onto the tubercle of the supinator crest of the ulna.
O’Driscoll and associates5 first described posterolateral instability of the elbow in 1991. The cause was thought to be LUCL laxity, which allows for rotatory subluxation of the ulnohumeral joint and, subsequently, a secondary dislocation of the radiocapitellar joint. The LCL complex maintains these joints in a reduced position when the elbow is loaded in supination. However, a mechanism for elbow subluxation and dislocation has been described in which there is increased ligamentous and capsular damage, progressing from lateral to medial across the joint. Elbow dislocation is the final of the three sequential stages of instability from posterolateral rotation. The lateral complex also resists varus forces.
Dynamic stability. The flexor and extensor muscles achieve compression across the elbow joint and, in turn, provide dynamic stability. In addition, the extent of instability after a simple elbow dislocation appears to be directly associated with the amount of muscle damage on both the medial and lateral epicondyles. The brachialis and triceps also provide stability, particularly because they have broad cross-sectional areas and also because their insertion is closer to the joints and pivot of joint rotation. Overall, muscle instability is likely, but the magnitude and effect are uncertain.
Medial instability
Recurrent medial instability usually is associated with chronic overuse from sports activities, such as those that involve overload throwing. Valgus stress is applied during throwing, resulting in repetitive microtrauma, attenuation, and even possible rupture to the MCL.6 Acute MCL ruptures may occur with elbow dislocations. They usually heal well, but in athletes there is a greater amount of valgus stress imposed on the elbow than in patients who have a dislocation and use the elbow for activities of daily living.
During the overhead throwing motion, valgus stress occurs primarily during the late arm-cocking and early acceleration phases. A significant amount of force may be generated but is dissipated through a combination of the MCL, flexor pronator mass, and ulnohumeral articulations. Acute ruptures of the MCL usually cause a “popping†sensation and pain and swelling over the medial aspect of the elbow.6
Presentation. Patients who have medial elbow instability usually present with pain and tenderness over the medial aspect of the elbow that is aggravated during and after throwing. If there is a ligament tear, pain may not occur until as much as 70% to 80% of the throwing effort has been made.7
Ulnar nerve symptoms also may occur with medial instability because of compression caused by inflammation of ligaments within the cubital tunnel or because of traction resulting from repeated valgus loading. Up to 40% of patients with medial instability have ulnar nerve symptoms.8, 9
Patients may have point tenderness over the insertion of the anterior bundle of the MCL, which is 2 cm distal to the medial epicondyle. Elbow motion usually is not compromised and elbow instability may be difficult to demonstrate.
Testing. Norwood and colleagues6 described an abduction stress test as a means of evaluating MCL integrity. The test is performed with the forearm supinated and in 15º to 20º of elbow flexion to unlock the olecranon from its fossa. Any reproduction of the athlete’s symptoms is a positive test result. It is currently recommended that the test be performed with the patient’s forearm in full pronation-supination, because a pseudovalgus instability may occur as a result of unrecognized posterolateral instability.10
The moving valgus stress test may be more sensitive in the evaluation of injury to the MUCL. The shoulder is abducted to 90º and fully externally rotated to recreate the throwing position. The elbow is then flexed and extended with a valgus force applied. Pain directly over the MUCL is considered a positive test result. This is the most useful clinical examination in our hands.
The milking maneuver requires the patient to reach under the affected arm, grab the thumb, and pull the elbow into valgus. Pain over the MUCL is considered a positive result. Very few of our patients can perform this maneuver.
These tests apply a valgus stress to the elbow during extension and flexion in an attempt to elicit pain and demonstrate joint line opening. Deficiency of the anterior bundle of the MCL during these tests has been shown to be significantly greater at 70º of flexion than at 30º. Therefore, clinical testing should be performed at these higher degrees of flexion. Detection of partial ruptures of the anterior bundle based on medial joint line opening and increased valgus movement usually is not possible.
Imaging. Recurrent medial instability is primarily a clinical diagnosis, but a stress radiograph may help confirm the diagnosis. However, a normal x-ray film result does not rule out symptomatic ligament attenuation. Stress radiography may be performed with gravity or manually. Plain radiographs also may demonstrate abnormalities associated with recurrent MCL instability, including medial olecranon osteophytes, loose bodies, ligamentous calcification, and formation of heterotopic bone.
Stress radiography results should be compared with those from the contralateral side, because significant ulnohumeral gapping may occur in persons who have normal elbows. For overhead throwers, a side-to-side difference greater than 2 mm is a good standard for making the diagnosis of MCL insufficiency.
MRI is the modality of choice for evaluating MCL insufficiency. Diagnosis of partial tears on MRI is more difficult. Because these partial tears usually occur in the under surface of the ulnar attachment of the MCL, use of MRI with intra-articular gadolinium may provide information for making a diagnosis of partial MCL tears. The role of ultrasonography in evaluation remains to be determined.
Lateral instability
 Patients who have lateral instability usually present with symptoms after an elbow dislocation. In some cases, there may be a history of lateral-side surgery.
Patients who have lateral instability usually present with symptoms after an elbow dislocation. In some cases, there may be a history of lateral-side surgery.
Presentation. The clinical presentation varies, but typically the patient has a history of painful clicking, catching, or snapping of the elbow; there may be a sensation that the elbow is slipping in and out of the joint. Symptoms typically occur in the extension portion of the motion arc with the forearm in supination. Those that occur with flexion and pronation probably are related to reduction of the subluxation. The classic activity that patients report that will reproduce their symptoms is rising from a chair while pushing down on the arm rest. Motion usually is normal, but patients may be apprehensive in full supination and extension.
Testing. The test reported to be most sensitive is a lateral pivot shift apprehension test.8 The test is performed with the patient prone or supine. The forearm is fully supinated, and valgus force is applied while it is moved back to full extension. The radial head and proximal lateral forearm are noted to shift posterolaterally and then reduced similar to the same test in the anterior cruciate ligament–deficient knee. Posterolateral instability is best detected between 70º and 110º of flexion.
Two other clinical tests described by Regan involve having the patient push up from a chair but with the palms facing inward, and having the patient push up from a prone position first with the forearms maximally pronated and the thumbs pointing toward each other. Repeating the test with the thumbs pointed outward and the forearms maximally supinated elicits symptoms that were not present with the forearms pronated. This test may be performed with the patient standing and performing a wall push-up.11
Imaging. Plain radiography results usually are normal, but stress radiographs may help the diagnosis. MRI also may help in the diagnosis of posterolateral instability, and adding gadolinium may allow for clear depiction of the undersurface tears, which are poorly demonstrated on a conventional MRI scan.
Manish A. Patel, MD, practices orthopedic surgery and sports medicine at Southampton Orthopaedic and Sports Medicine Center in Franklin, VA. Felix H. Savoie III, MD, is the Lee Schlesinger professor of shoulder, elbow, and sports surgery at Tulane University School of Medicine in New Orleans.A version of this article originally appeared in our sister publication, the Journal of Musculoskeletal Medicine, in May.
References
1. Morrey BF, An KN. Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med 1983;11(5):315-319.
2. An KN, Morrey BF, Chao EY. The effect of partial removal of proximal ulna on elbow constraint. Clin Orthop Relat Res 1986;209:270-279.
3. Regan W, Morrey B. Fractures of the coronoid process of the ulna. J Bone Joint Surg 1989;71A(9):1348-1354.
4. Safran M, Ahmad CS, Elattrache NS. Ulnar collateral ligament of the elbow. Arthroscopy 2005;21(11):1381-1395.
5. O’Driscoll SW, Morrey BF, Korinek S, An KN. Elbow subluxation and dislocation: a spectrum of instability Clin Orthop Relat Res 1992;280:186-197.
6. Norwood LA, Shook JA, Andrews JR. Acute medial elbow ruptures. Am J Sports Med 1981;9(1):16-19.
7. Fleisig GS, Andrews JR, Dillmon CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med 1995;23(2):233-239.
8. Conway JE, Jobe FW, Glousman RE, Pink M. Medial instability of the elbow in throwing athletes: treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg 1992;74A(1):67-83.
9. Andrews JR, Timmerman LA. Outcome of elbow surgery in professional baseball players. Am J Sports Med 1995;23(4):407-413.
10. Armstrong AD, Dunning CE, Ferreira LM, et al. A biomechanical comparison of four reconstruction techniques for the medial collateral-deficient elbow. J Shoulder Elbow Surg 2005;14(2):207-215.
11. Regan W, Lapner PC. Prospective evaluation of two diagnostic apprehension signs for posterolateral instability of the elbow. J Shoulder Elbow 2006;15(3):344-346.
